The Role of Imaging in Diagnosing Osteoid Osteoma
Osteoid osteoma is a relatively rare but painful bone tumour that primarily affects young adults and adolescents. While it’s benign in nature, its symptoms can be debilitating. A crucial step in the management of osteoid osteoma is accurate diagnosis, and imaging plays a central role in achieving this goal. In this article, we will explore the significance of imaging techniques in diagnosing osteoid osteoma and their role in guiding treatment decisions.
Understanding Osteoid Osteoma
Osteoid osteoma is a benign bone tumour that typically arises in the long bones, with the femur and tibia being the most common locations. It is characterised by a small, painful, and benign nidus (centre) surrounded by a reactive bone. The tumour causes localised pain, often worse at night, which can be severe and persistent. Patients with osteoid osteoma treatment may also experience limited joint mobility or muscle atrophy due to pain and inflammation.
Diagnosing osteoid osteoma based solely on clinical symptoms and physical examination can be challenging, as the pain can mimic other musculoskeletal conditions. Therefore, the role of advanced imaging modalities is pivotal in confirming the diagnosis and facilitating appropriate treatment.
Imaging Techniques for Diagnosing Osteoid Osteoma
Several imaging modalities are used to diagnose osteoid osteoma treatment, each with its own advantages and limitations. These techniques help visualise the tumour’s location, size, and characteristics, aiding in the accurate diagnosis of this condition.
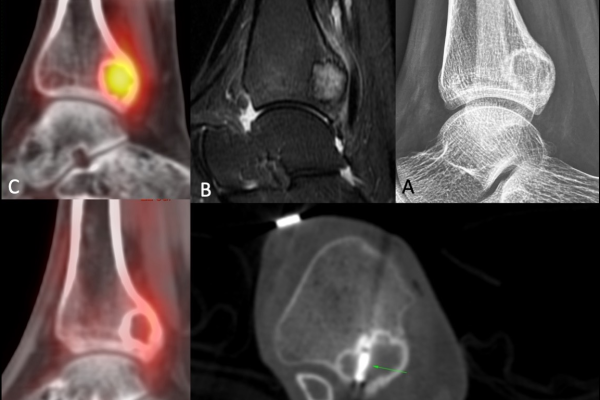
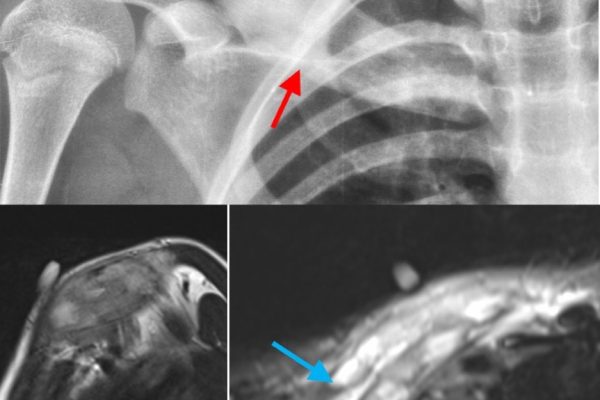
X-rays: X-rays are often the initial imaging study performed when osteoid osteoma is suspected. On an X-ray, the tumour appears as a small, well-defined radiolucent nidus surrounded by reactive sclerotic bone. While X-rays provide essential information, they may not always reveal the tumour, particularly in the early stages when it is small and less calcified.
Computed Tomography (CT) Scans: CT scans are highly effective in detecting osteoid osteoma, especially when X-rays are inconclusive. CT scans provide detailed cross-sectional images of the bone and can precisely locate the tumour, helping surgeons plan for minimally invasive treatments like radiofrequency ablation (RFA). The nidus is typically seen as a central radiolucent area surrounded by a dense sclerotic reaction on CT images.
Magnetic Resonance Imaging (MRI): MRI is another valuable imaging tool in diagnosing osteoid osteoma, particularly when the tumour is near joints or in areas where a CT scan might not provide the best visualisation. MRI can help assess soft tissue involvement, which is crucial for surgical planning. On MRI, the nidus typically appears hypointense on T1-weighted images and hyperintense on T2-weighted images.
Technetium Bone Scans: Bone scans using technetium-99m-labelled diphosphonates can help identify areas of increased bone turnover, which can be indicative of osteoid osteoma. However, this method is less specific and may require further imaging for confirmation.
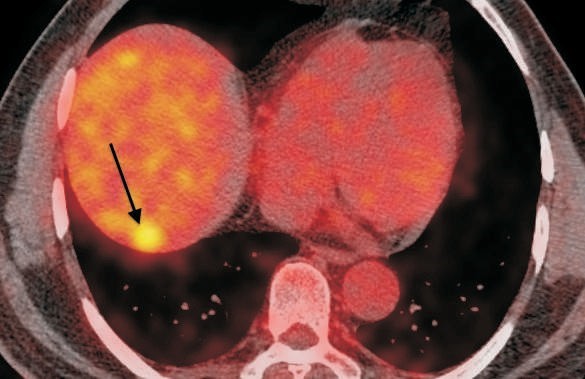
Positron Emission Tomography (PET) Scans: PET scans are not typically used as a first-line diagnostic tool for osteoid osteoma, but they can be useful in certain cases, especially when other imaging results are inconclusive. PET scans can detect areas of increased metabolic activity, which may be present in some osteoid osteomas.
Treatment Guidance
Once osteoid osteoma is accurately diagnosed through imaging, appropriate treatment options can be considered. The two main treatment approaches for osteoid osteoma are surgical excision and minimally invasive techniques like radiofrequency ablation (RFA).
Surgical Excision: Traditional surgery involves the complete removal of the tumour, which can be highly effective. However, it may require a larger incision, longer recovery time, and potential complications.
Radiofrequency Ablation (RFA): RFA has become the preferred treatment option for many patients with osteoid osteoma. This minimally invasive procedure involves using imaging guidance to precisely target and ablate the tumour with heat. RFA offers several advantages, including smaller incisions, shorter recovery periods, and less post-operative pain.
Imaging plays a pivotal role in guiding the choice between surgical excision and RFA. CT scans and MRIs are especially useful in this regard, as they help surgeons assess the size, location, and soft tissue involvement of the tumour. RFA is typically recommended for tumours that are easily accessible and less than 3 cm in size.
Conclusion
In the diagnosis and management of osteoid osteoma, advanced imaging techniques are indispensable. X-rays, CT scans, MRIs, bone scans, and, in some cases, PET scans all contribute to the accurate identification of the tumour’s location and characteristics. These imaging modalities are not only essential for confirming the diagnosis but also for guiding treatment decisions. Whether it’s surgical excision or minimally invasive RFA, the choice of treatment often depends on the information gleaned from these imaging studies. Early and accurate diagnosis, facilitated by imaging, is key to providing effective relief for patients suffering from osteoid osteoma and improving their quality of life.