Radiofrequency Thermal Ablation of Osteoid Osteomas
Radiofrequency Thermal Ablation of Osteoid Osteomas
An osteoid osteoma is a benign bone neoplasm that occurs typically in the long bones, such as the tibia or the fibula in about 50% of cases, in the diaphyseal or meta-diaphyseal cortex (Fig. 1). It is a relatively common neoplasm, representing about 12% of all primary bone neoplasms.
The typical age group is between 5 and 25 years of age (>75%) and more common in men. Patients with osteoid osteomas typically have pain, which become worse at night and which responds to anti- inflammatory drugs.
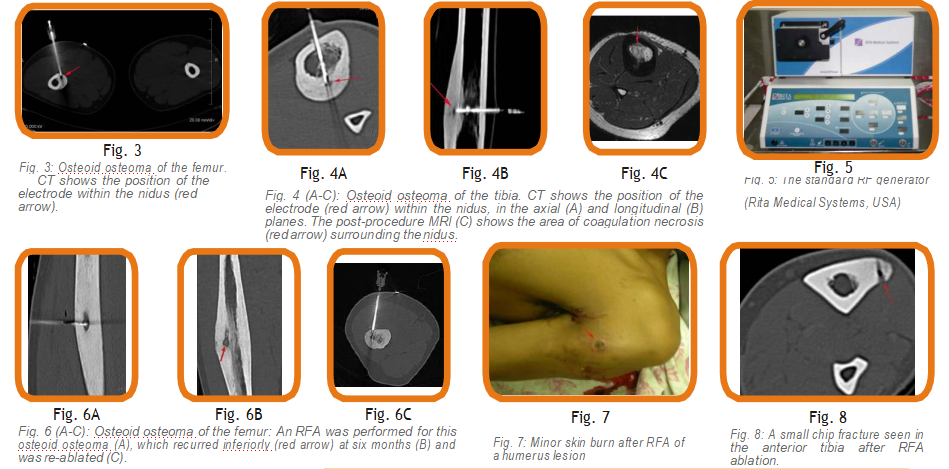
Radiologically, an osteoid osteoma has a typical appearance of cortical thickening and sclerosis. A nidus may not always be seen on plain radiographs, but will always be identified on CT (Fig. 1). On MRI, there is marrow edema with perisseous edema and usually the nidus is well visualized (Fig. 2).
Traditionally, an osteoid osteoma has been treated with en-bloc resection and surgery. Though the results are good (85-95%), the complication rates are high, including fracture at the site of excision.
Among other alternative techniques is radiofrequency ablation (RFA). The principle of RFA is to induce thermal coagulation in the lesion and to “cook” the lesion to death. Cure rates with RFA are between 80- 90%, with a 100% cure rate for a second sitting, if the lesion recurs. The complication rate is less than 2%.
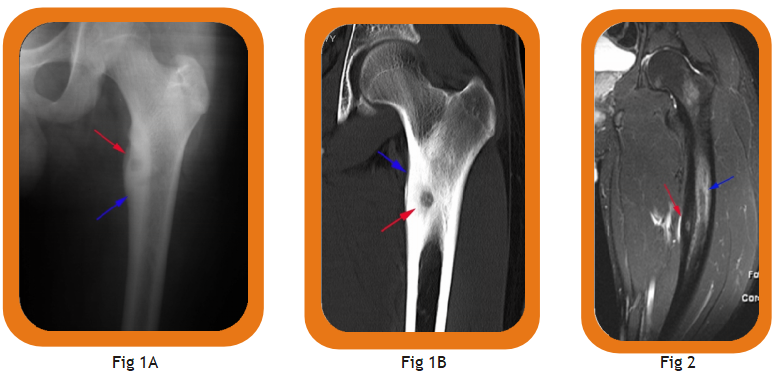
Fig. 1 (A, B): Osteoid osteoma. Plain radiograph (A) and CT (B) showing a typical meta-diaphyseal, cortical osteoid osteoma involving the upper end of the femur. The nidus is well seen (red arrow) with the surrounding cortical thickening (blue arrow).
Fig. 2: Osteoid osteoma. MRI shows the nidus (red arrow) along with marrow edema (blue arrow).
Method:
The procedure is performed on an outpatient basis. After the lesion has been localized, deep sedation is given. A bone-biopsy trephine needle is inserted into the nidus. Through this needle, the RFA electrode is introduced (Figs. 3, 4). A standard RF generator is used (Fig. 5). A temperature of approx. 100 degrees Celsius is applied for 5 minutes. If necessary, this cycle is repeated once more.
Technical success is defined as the ability to put the These included the femur (22), tibia (5), fibula (1), RFA electrode into the nidus. Clinical success is defined as absence of pain after 24 hours following the procedure.
The patient is discharged the moment the effect of the anesthesia has worn-off and the patient has regained consciousness. A post-procedural course of antibiotics and anti-inflammatory drugs is prescribed.
Materials:
The procedure was performed on 31 patients. These included the femur (22), tibia (5), fibula (1), humerus (1), radius (1) and patella (1).
Results:
All patients were pain-free within 48 hours. The follow-up time has ranged from 2-20 months. One patient has had recurrence, which occurred after 3 months and the procedure was repeated six months after the first procedure
Minor complications occurred in two patients (11%), consisting of a localized superficial skin burn (Fig. 7) and a small chip fracture (Fig. 8).
Complications
- Thermal burns due to improper grounding or electrode placement
- Procedural pain and discomfort
Contraindications
- Lesions within 1cm of a major neurovascular bundle
- Inability to withstand deep sedation
Discussion
On CT, there are no immediate signs of cure. In about 50% of patients, the lesion undergoes complete sclerosis at the end of six months, partial sclerosis in another 25% and no change in 25%. Therefore procedure success is purely measured on clinical grounds; i.e. disappearance of the typical pain associated with the lesion. On MRI, marrow edema is often seen around the site of ablation, demarcating
the area of coagulation necrosis (Fig. 4C).
Conclusion
RFA is perhaps the best way to treat, if technically possible. The method is safe, effective and avoids major surgery and thus significant morbidity.